Tendonitis Palos Hills, Mokena and Chicago
Tendons connect muscle to bone and are primarily made up of collagen fibers, water, and connective tissue. They are an integral component of our musculoskeletal system, but can be a source of pain, dysfunction and may lead to a condition called tendonitis.
Tendon problems (or tendinopathy) may affect any joint, especially the shoulder, elbow, wrist, hip, knee, ankle, etc. As with a muscle, tendons have structural breaking points. When stress is applied to the tendon, it will elongate slightly.
If the stress continues beyond the tensile strength that the tendon can handle, it will rupture. This frequently requires surgical treatment and should be evaluated by a physician if suspected.
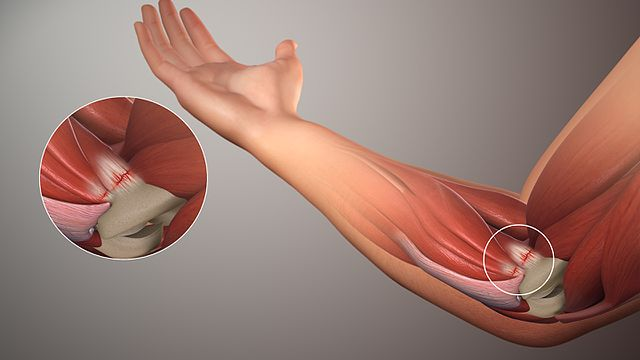
Not all tendinopathies result in catastrophic failures or ruptures, however. Tendonitis is the inflammation of a tendon, and is a common overuse injury.
Tendonitis can happen to anyone at any age and activity level, but more commonly affects athletes and other physically active adults. This frequently occurs in the achilles, patellar, hamstring, wrist extensor, biceps/triceps, and rotator cuff tendons.
While less common, it may also occur in the hips and torso, or other joints in the body.
Symptoms & Causes
Symptoms of tendonitis may consist of:
- activity related pain around the area
- joint stiffness
- swelling, redness, and tenderness surrounding the site
- burning sensation surrounding the affected area
Joint pain is often worse during or after physical activity and may result in stiffness the following morning caused by tightened muscles around the inflamed tendon. While tendonitis is an inflammatory problem in its acute form, prolonged symptoms may be diagnosed as “tendinosis,” a more severe condition that often represents a lack of biologic healing response necessitating different treatments.
Common causes of tendonitis include:
- Overuse, or improper exercise techniques
- Manual labor
- Sports
- Structural abnormalities
- Training surfaces that do not “give” to muscles
Classifications
There are six classifications of tendonitis ranging from mild to severe. These classifications are determined by the degree of pain experienced by the patient before, during, and after exercise and is correlated to the patient's overall physical functionality.
- Mild tendonitis (stages 1-2) - Pain is caused by extreme exertion that ceases when activity stops. Patients can often exercise, work, or compete with mild tendonitis without severe repercussions.
- Moderate Tendonitis (stages 3-4) - Pain is caused by extreme exertion that lasts for several hours after physical activity has stopped. When pain severity is approaching stage 4, normal functioning is impaired.
- Severe Tendonitis (Stage 5-6) - Intense pain occurs during physical activity and long after the activity stops, sometimes lasting for days and not associated with any extreme exertion. Severe tendonitis affects normal day-to-day function for working adults and athletes and requires medical attention.
Common Misconceptions
Despite the commonality of this condition, there is abundant misinformation regarding the causes and treatment of tendonitis.
Myth #1: Rest is Best
While resting the inflamed tendon is often necessary to calm the inflammation, prolonged rest can actually weaken the tendon and lead to stiffness which may worsen the pain. When experiencing tendonitis, the goal is to find a tolerable load that does not exacerbate the problem, but continues to build the capacity of the tendon, and maintain the health of the surrounding muscles/joints. If the patient rests for too long before returning to the same activity level, that will spike the load on the tendon, which increases the likelihood of re-injury.
![image2]() Myth #2: Stretching will Help the Problem
Myth #2: Stretching will Help the Problem
While it is true that tight muscles contribute to tendon pain, improper stretching may actually cause further harm, so it is often useful to be under the treatment and supervision of a trained physical therapist. Compressing the tendon against bone often leads to more irritation, which can damage the overall structure of the tendon.
Newer, alternative techniques such as the use of a foam roller or lacrosse ball to massage the affected area as it can relax the muscle without further tendon compression. These should be directed by a physician and/or therapist in the beginning.
Myth #3: Tendonitis is Caused by Inflammation
Inflammation is not the primary driver of tendonitis. The inflammation and subsequent tendonitis is secondary to mechanical overloading and the inflammation is a result thereof. Although this may seem trivial, it does affect how doctors treat the condition. Treatment relies less on NSAIDs solely as a long-term treatment option, and rather focus on changing the mechanical workload on the tendon as well.

Treatment
The first step when treating tendonitis is to get the inflammation under control. Cease doing the activity that caused the initial injury whether it’s sports, manual labor, or exercise. Many doctors will recommend the PRICE principle when treating tendon pain: Protection, Rest, Ice, Compression and Elevation.
NSAIDs may be prescribed for pain management and inflammation control. Rest is crucial during the initial phase of healing, and if not adhered to, may create further complications down the line.
As pain and swelling dissipate, the patient can progressively work to improve their range of motion and strengthen the injured tendon. Flexibility exercises should focus on elongating the tendon without increasing overall pain. Strengthening exercises should be light in intensity and high in repetition so as not to place excessive stress on the tendon.
Physical therapy or occupational therapy may also be recommended. Some patients see improvement as soon as 2-3 days from the initial injury, while full recovery for more severe cases can last anywhere from 3-6 months.

Dr. Adam F. Meisel
For specialized care in tendonitis treatment, turn to Dr. Adam F. Meisel, MD. Dr. Meisel is the Sports Medicine specialist at MidAmerica Orthopaedics, and is active in researching topics such as meniscal tears, ankle cartilage injuries, and cartilage transplants. Dr. Meisel studied Sports Medicine and Arthroscopy at the Southern California Orthopaedic institute, where he was provided with extensive training in caring for the shoulder, hip, knee, ankle, as well as treatments involving tendons, ligaments, and cartilage injuries.
To learn more about MidAmerica Orthopaedics and the different treatment options available to you, visit our website.
To schedule an appointment with MidAmerica Orthopaedics Dr. Adam F. Meisel or any of our other providers, call (708) 237-7200.

 Myth #2: Stretching will Help the Problem
Myth #2: Stretching will Help the Problem