Physical Medicine & Rehabilitation
What is Physical Medicine and Rehabilitation?
Physical Medicine and Rehabilitation (PM&R) physicians, also known as physiatrists, evaluate and treat injuries, illnesses, and disability, and are experts in designing comprehensive, patient-centered treatment plans. Their goal is to decrease pain and enhance performance without surgery.
PM&R physicians treat a wide variety of medical conditions affecting the brain, spinal cord, nerves, bones, joints, ligaments, muscles, and tendons. Physiatrists utilize cutting-edge as well as time-tested treatments to maximize function and quality of life.
Conditions & Treatments
PM&R physicians (or physiatrists) evaluate and treat patients with short- or long-term physical and/or cognitive impairments and disabilities that result from musculoskeletal conditions (neck or back pain, or sports or work injuries), neurological conditions (stroke, brain injury or spinal cord injury) or medical other conditions.
Physiatrists Perform
Especially in the inpatient setting, physiatrists provide general medical treatment similar to internal medicine to maintain medical stability and provide secondary prevention of disability. Physiatrists do not perform surgery, yet have many procedural opportunities for diagnosis and treatment. Many of these procedures may require fellowship or advanced training to perform.
EMG (Electromyography)
The inserting of fine needle electrodes in muscles and observing the recorded motor unit potentials when the muscles are activated to help distinguish whether weakness is due to muscle or nerve dysfunction (i.e., myopathy vs. neuropathy).
NCS (Nerve Conduction Studies)
The use of electrodes to record motor and sensory responses that are propagated by electrical stimuli. This test can help distinguish location of a nervous system lesion (radiculopathy, peripheral neuropathy, motor neuron disease, or neuromuscular junction).
Peripheral Joint Injections
Injections to help diagnose and treat bone and soft tissue disorders often seen in orthopedic, rheumatologic, and sports medicine disorders such as knee osteoarthritis, rotator cuff tendinopathy, and epicondylitis.
Trigger Point Injections
Lidocaine or dry needling can be used as an adjunct to proper exercise and physical therapy to treat trigger points, thought to be sources of chronic myofascial (soft-tissue) pain.
Musculoskeletal Ultrasound
Although it has been used for decades as a modality to deliver deep heat in therapies, ultrasound is now increasingly being used in the outpatient setting to supplement the musculoskeletal evaluation. Ultrasound may be used to evaluate for soft tissue abnormalities in commonly examined joints and structures. This technology is also now frequently used to guide injections, as it allows for improved placement of needles for delivery of treatment without exposure to ionizing radiation.
Spasticity Management
Spasticity is a common complication related to central nervous system (CNS) injury (e.g., SCI, stroke, cerebral palsy). Physiatrists treat spasticity by using oral antispasticity agents, botulinum toxin injections, phenol injections, and intrathecal baclofen pump management to improve function and decrease pain.
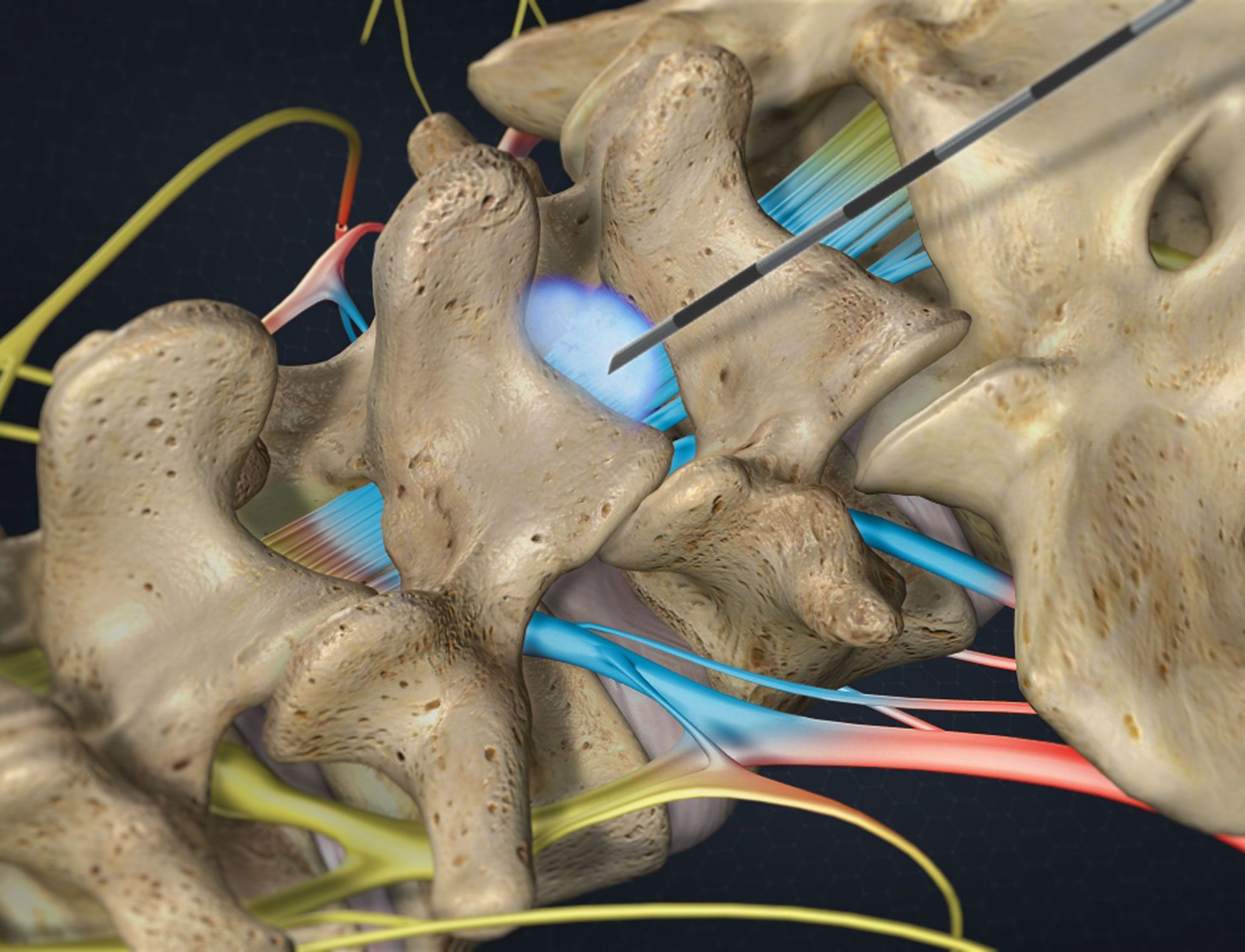
Interventional Spinal Therapeutics
Image-guided spinal diagnostics and injections, including:
- discograms
- interlaminar and transforaminal epidurals
- radiofrequency ablations
- spinal cord stimulation
- vertebroplasty
- kyphoplasty
- intrathecal pump placements
These techniques are being used as a non-surgical pain-relieving intervention for back pain and radiculopathy.
Additional Procedures
Other procedures performed by some physiatrists include:
- acupuncture
- prolotherapy
- platelet rich plasma injections
- autologous stem cell treatments